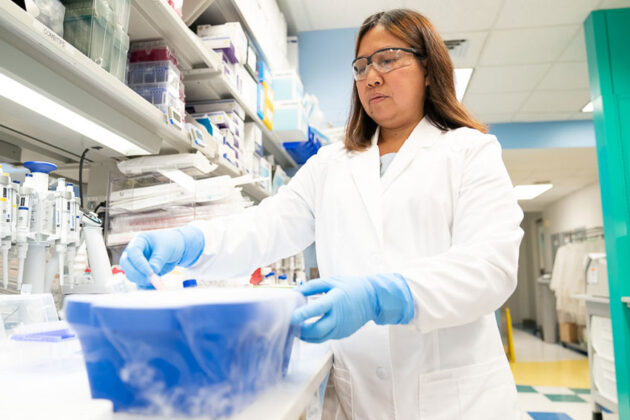
Marker Therapeutics is dedicated to the development and commercialization of next-generation T cell-based immunotherapies for patients with a wide range of blood and solid tumor cancers. Our team is comprised of talented and passionate professionals with deep expertise in cancer immunotherapy and driven by an urgency to deliver effective treatments to patients who currently have few or no therapeutic options.
Leveraging our novel MultiTAA technology – which uses non-genetically engineered T cells designed to recognize and kill multiple tumor targets – we believe we can develop more precise and safer therapies capable of resulting in broad, potent and durable anti-cancer activity. To date, our technology has been studied in hundreds of patients with various forms of hematological cancers and solid tumors in investigator-sponsored studies led by our partners at the Baylor College of Medicine. These results demonstrated the broad potential of our platform and informed our decision to initiate our first Company-sponsored study in post-transplant acute myeloid leukemia, or AML. We are currently enrolling patients in the safety lead in portion of our multicenter randomized Phase 2 AML study.